Parkinson’s disease is one of the most challenging neurological conditions known in medicine, affecting movement, behavior, and quality of life. When someone is diagnosed, one of the most pressing and emotional questions they and their families face is: Will Parkinson’s disease kill you? The answer is complex, but understanding it begins with how the disease works, progresses, and interacts with the body over time. While Parkinson’s disease itself is not directly fatal, the complications it causes can become life-threatening. Awareness, proactive treatment, and lifestyle management can make a significant difference in lifespan and quality of life.
Understanding Parkinson’s Disease
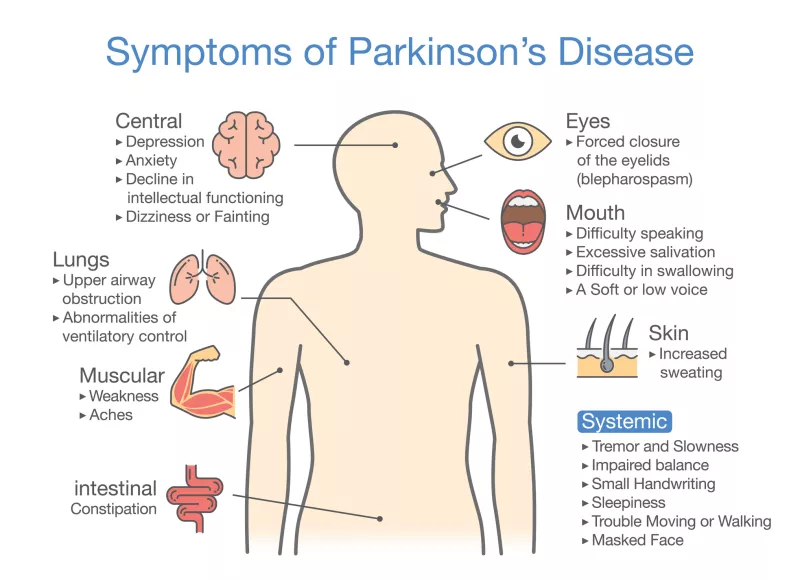
Parkinson’s disease is a chronic, progressive disorder of the nervous system that primarily affects movement. It occurs when nerve cells in the brain, specifically in an area called the substantia nigra, begin to break down or die. These cells produce dopamine, a chemical that helps coordinate muscle movement. When dopamine levels drop, it leads to the characteristic symptoms of Parkinson’s:
- Tremors, typically in the hands, arms, or legs
- Muscle stiffness or rigidity
- Slowness of movement (bradykinesia)
- Impaired balance or coordination
- Shuffling walk or stooped posture
Although the condition starts with physical symptoms, it can also affect mental and emotional health over time. Anxiety, depression, and cognitive changes are common as the disease progresses.
How Parkinson’s Affects Longevity
The most important fact to understand is that Parkinson’s disease itself is not considered directly fatal. Unlike diseases such as cancer or heart failure, the main problem in Parkinson’s is the gradual loss of motor control and the complications that come from long-term disability. Many people live with Parkinson’s for decades after their diagnosis, managing symptoms effectively through medication, therapy, and support.
The average life expectancy for someone with Parkinson’s today is only slightly shorter than that of the general population. In other words, most people with Parkinson’s do not die from the disease, but rather with it.
What Actually Causes Death in Parkinson’s Patients?
While Parkinson’s does not directly shut down organs or destroy vital systems, its secondary effects can lead to serious health challenges. The most common causes of death related to Parkinson’s include:
- Aspiration pneumonia – difficulty swallowing can cause food or liquid to enter the lungs, leading to infection.
- Falls and injuries – loss of coordination and balance often increases the risk of falls, which can lead to fractures or head injuries.
- Complications from immobility – reduced movement can cause circulation issues, blood clots, or infections.
- Cardiovascular or respiratory complications – as the nervous system changes, the body’s automatic functions (like breathing and heartbeat) can be affected.
- Side effects of medications or advanced treatments – these, though rare, can also contribute to complications if not monitored properly.
Managing these risks is the key to living longer with Parkinson’s. Medical care, proper nutrition, exercise, and psychological support can all extend life expectancy significantly.
Stages and Progression of Parkinson’s Disease
Parkinson’s disease typically progresses through five stages, each presenting different levels of challenge and care needs.
- Stage 1: Mild symptoms. Tremors or small movement changes occur, often on one side of the body. Daily life remains mostly unaffected.
- Stage 2: Symptoms worsen and affect both sides, though balance is maintained. Everyday tasks start taking longer.
- Stage 3: Balance becomes more difficult, and falls are more frequent. Independence is still possible, but help may be needed for some activities.
- Stage 4: Severe symptoms limit mobility. Assistance is usually required for most daily activities.
- Stage 5: Advanced Parkinson’s leads to severe stiffness, immobility, and sometimes inability to speak or swallow well. Ongoing medical care and caregiver support become essential.
Even at advanced stages, medical treatment can help ease discomfort and extend life with dignity. People often live 15 to 30 years after Parkinson’s onset, particularly when diagnosed early and treated thoroughly.
Does Early Diagnosis Improve Survival?
Absolutely. Early detection allows doctors to begin treatments that slow progression and reduce complications. Medication like levodopa and dopamine agonists can restore dopamine balance, improving motor control. Regular monitoring allows for adjustments before severe disability sets in.
Treatment doesn’t stop at medication. Early-stage patients benefit most from a multidisciplinary approach that includes:
- Physical and occupational therapy
- Speech and swallowing therapy
- Nutritional counseling
- Mental health support
These interventions delay disability and lower the risk of fatal complications later in life.
The Role of Exercise and Lifestyle
What’s remarkable about Parkinson’s research is the growing evidence that lifestyle habits play a powerful role in longevity. Regular exercise, in particular, stands out as a proven way to slow progression and maintain body function.
Physical activity such as walking, swimming, yoga, and resistance training can:
- Improve balance and muscle strength
- Enhance mood and sleep
- Support cardiovascular health
- Reduce constipation and stiffness
- Improve medication absorption and effectiveness
Diet also plays an important role. A balanced meal plan rich in antioxidants, omega-3 fatty acids, and fiber helps the brain and body better resist the effects of Parkinson’s. Hydration prevents medication side effects and supports mobility.
Emotional and Cognitive Health in Parkinson’s
Depression, anxiety, and cognitive decline often accompany Parkinson’s because dopamine also affects mood and cognition. Emotional support is not only about comfort—it is directly tied to physical health. Untreated depression can lower energy, reduce exercise, and worsen outcomes. Mental resilience improves the ability to manage day-to-day life and medication schedules.
Therapies like cognitive-behavioral therapy (CBT), mindfulness-based stress reduction, and community support groups can strengthen emotional well-being, helping patients live meaningfully and avoid decline from inactivity or stress-related complications.
Modern Treatments That Improve Survival
Advances in medicine have dramatically changed the prognosis for people with Parkinson’s. Today, several effective therapies exist to manage symptoms and maintain independence:
- Levodopa-Carbidopa: The gold-standard medication that replenishes dopamine.
- Dopamine agonists and MAO-B inhibitors: Extend dopamine function or slow its breakdown.
- Deep brain stimulation (DBS): A surgical technique that delivers electrical impulses to specific brain regions, improving movement control.
- Focused ultrasound therapy: A non-invasive method for controlling tremors.
- Continuous drug infusions: Used for advanced Parkinson’s when oral medication fluctuates.
Because of these innovations, patients diagnosed in their 50s or 60s often live well into their 80s with proper care. Early medical consultation and personalized treatment plans remain the most critical steps in preventing fatal complications.
The Importance of Ongoing Medical Care
Regular check-ups with a neurologist are crucial in detecting side effects early, adjusting medications, and preventing emergencies. Many patients also benefit from coordinated care involving physiotherapists, speech therapists, dietitians, and mental health counselors.
Ignoring symptom progression or stopping medication abruptly can lead to severe muscle rigidity, confusion, or infection—all of which can become life-threatening if untreated.
How Families and Caregivers Can Help
Families play an enormous role in Parkinson’s survival outcomes. Loved ones can assist by:
- Maintaining consistent medication timing and tracking dosages.
- Monitoring for swallowing issues or aspiration risk.
- Helping with mobility, reducing fall risks at home.
- Encouraging emotional support and social activity.
Caregiver burnout is also common, so support networks and respite care are essential for both patient and caregiver well-being.
Can Parkinson’s Disease Be Prevented?
While no guaranteed prevention exists, research is identifying potential protective factors. Regular exercise, a diet rich in fruits and vegetables, and limiting exposure to toxins like pesticides may lower risk. Some studies also suggest that caffeine, green tea, and certain dietary antioxidants may help reduce the likelihood of developing Parkinson’s, though more evidence is needed.
Living Well Despite Parkinson’s
Many people live fulfilling, long lives despite Parkinson’s. Public figures such as Michael J. Fox and Muhammad Ali brought global attention to the disease, demonstrating that a strong will, medical care, and lifestyle management can overcome many challenges. Support, positivity, and medical advances continue to redefine what it means to live with Parkinson’s.
Maintaining optimism, social connection, and mental engagement—through hobbies, volunteering, or learning—has measurable benefits for both mood and longevity. The disease may change how a person moves, but it does not necessarily define or dictate how long they live.
Key Takeaway: Parkinson’s Disease Does Not Have to Be a Death Sentence
So, will Parkinson’s disease kill you? Most often, the answer is no. It rarely causes death directly. What matters most is how the disease is managed—the attention given to therapy, diet, exercise, emotional health, and medical follow-ups.
While it is a progressive condition with no cure yet, today’s treatments offer hope and control. People are living longer than ever with Parkinson’s, maintaining independence and quality of life for decades after diagnosis.
Living with Parkinson’s demands awareness, support, and patience, but it is far from hopeless. With proper medical oversight, healthy habits, and strong emotional resilience, Parkinson’s disease does not have to shorten life—it can instead redefine it with strength, adaptability, and purpose.

Leave a Reply