Epilepsy is a neurological condition where a person has a tendency to have recurrent, unprovoked seizures due to abnormal electrical activity in the brain. Seizures can look very different from person to person, ranging from brief staring spells to full‑body convulsions with loss of consciousness.
Common seizure types include generalized tonic‑clonic seizures (stiffening then jerking, loss of consciousness), focal seizures (starting in one area of the brain), and absence seizures (brief lapses in awareness). Knowing the person’s seizure type and typical pattern is essential for planning safety and first aid.
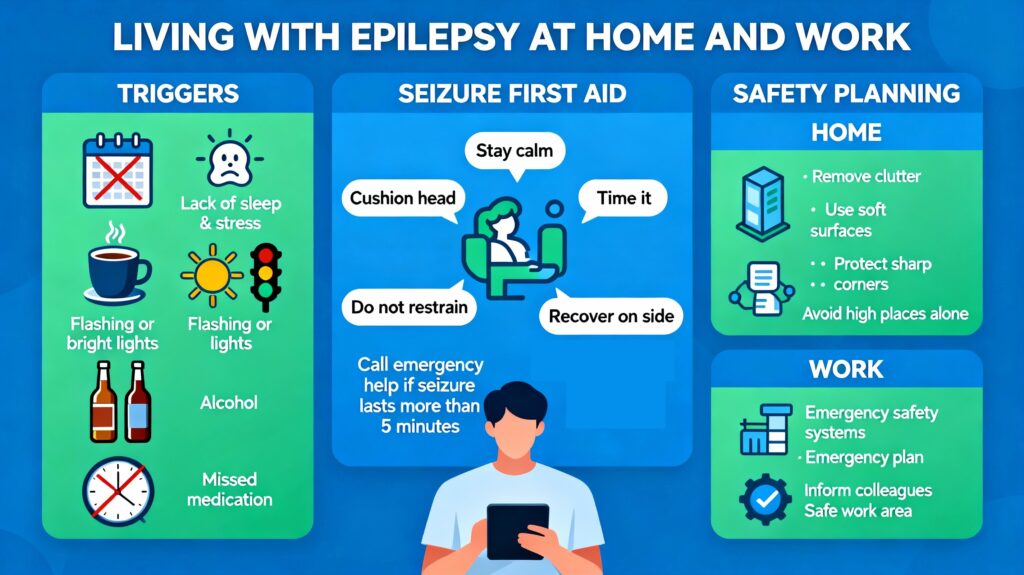
Common triggers and patterns
Not everyone with epilepsy has clear triggers, but many people notice patterns that can help with prevention. Tracking seizures in a diary or app makes it easier to spot personal triggers and share information with the treating neurologist.
Typical triggers to explore with a clinician include:
- Missed or late doses of anti‑seizure medication
- Sleep deprivation and irregular sleep patterns
- Fever, illness, or significant physical stress
- Alcohol, recreational drugs, or sudden withdrawal from them
- Flashing lights or visual patterns in light‑sensitive epilepsy
- Hormonal changes, including around menstruation
- High psychological stress or sudden emotional shocks
General safety principles
Good seizure management is about reducing risk, not eliminating all activity from daily life. The goal is to balance independence with sensible precautions tailored to the person’s seizure type, frequency, and warning signs.
Key safety principles include:
- Ensuring consistent medication use as prescribed and regular medical follow‑up
- Creating an individualized seizure and safety plan with a healthcare professional
- Sharing key information with trusted people at home, school, and work
- Avoiding high‑risk activities alone (heights, deep water, open flames, heavy machinery) if seizures are not fully controlled
Seizure first aid: what to do
Simple, calm first aid can prevent most seizure‑related injuries and complications. For most seizures, the focus is on keeping the person safe, protecting the airway, and staying with them until they recover.
For a generalized tonic‑clonic seizure:
- Stay calm and note the time when the seizure starts.
- Gently ease the person to the ground if they are standing and clear nearby hard or sharp objects.
- Place something soft under their head and loosen anything tight around the neck.
- Turn them gently onto their side when it is safe to do so to help keep the airway clear.
- Stay with them, speak calmly, and protect their privacy as they recover.
For focal or absence seizures, the person may not fall but can still be at risk of injury or confusion. In these situations, guiding them away from danger, helping them sit or rest, and staying with them until they are fully aware are often sufficient.
Seizure first aid: what not to do
Some widely held ideas about seizures are myths and can cause harm if followed. Avoiding these actions is as important as knowing what to do.
Do not:
- Put anything in the person’s mouth; this can break teeth or block the airway, and they cannot swallow their tongue.
- Restrain their movements or try to stop the jerking; this can cause injuries.
- Attempt mouth‑to‑mouth breathing during a convulsive seizure; focus on positioning and airway instead.
- Offer food, drink, or medication until the person is fully awake and able to swallow safely.
When to call emergency services
Most brief seizures end on their own and do not require an ambulance, but certain situations are emergencies. Clear criteria help bystanders act quickly when needed.
Seek urgent medical help (for example, call 911 or your local emergency number) if:
- A convulsive seizure lasts more than about 5 minutes or repeats without full recovery in between
- The person has trouble breathing or does not regain awareness after the seizure
- It is the person’s first known seizure or you are unsure if they have epilepsy
- The person is injured, pregnant, has diabetes, or the seizure happens in water
- You feel unable to keep them safe or follow the usual plan
Safety planning at home
Home is where many seizures occur, so small environmental changes can significantly reduce risk. The exact plan should be personalized with clinical advice, especially in families with children or frequent seizures.
Home safety ideas include:
- Using shower chairs, handheld shower heads, and avoiding locking bathroom doors so help can reach the person if they seize
- Adding non‑slip mats in bathrooms and kitchens and padding hard furniture edges in high‑risk areas
- Avoiding cooking over open gas flames alone if seizures are not fully controlled, or using back burners and lids when possible
- Keeping floors clear of clutter and securing loose rugs to reduce fall hazards
- Considering low beds or padded frames if night‑time seizures and falls from bed are a concern
Safety planning at work and school
With thoughtful planning and reasonable adjustments, many people with epilepsy can work and study safely and effectively. Open communication with employers or educators, when comfortable and appropriate, allows practical accommodations and training.
Important elements of a work or school plan:
- A written seizure action plan describing typical seizures, triggers, first‑aid steps, and when to call emergency services
- Identifying a few trained colleagues or staff who know how to provide seizure first aid
- Adjustments to tasks if seizures are uncontrolled in high‑risk roles (heights, driving, operating dangerous machinery)
- Flexible scheduling to accommodate medical appointments, medication side effects, or sleep needs if possible
Emotional and social aspects
Living with epilepsy often involves managing uncertainty, stigma, and changes in independence as much as managing seizures themselves. Access to counseling, peer support, and accurate education for family, friends, and coworkers makes a significant difference.
Useful strategies can include:
- Joining epilepsy support groups or online communities moderated by reputable organizations
- Involving family and close friends in appointments so they understand the condition and first aid
- Working with a mental health professional if anxiety, depression, or fear of seizures affects daily life
- Exploring legal protections and workplace or school rights for people with chronic conditions and disabilities in your region
Building your personal seizure plan
A personalized seizure and safety plan pulls together triggers, medications, first aid instructions, and emergency steps into one document. Many epilepsy organizations provide templates that can be filled out with a neurologist or epilepsy nurse.
Elements to include:
- Diagnosis and seizure types, usual frequency, and common triggers
- Current medications, doses, timing, and any rescue medications with instructions
- Step‑by‑step first aid for typical seizures, and clear criteria for calling an ambulance
- Contact details for emergency contacts and healthcare providers
- Workplace or school‑specific instructions where relevant

Leave a Reply