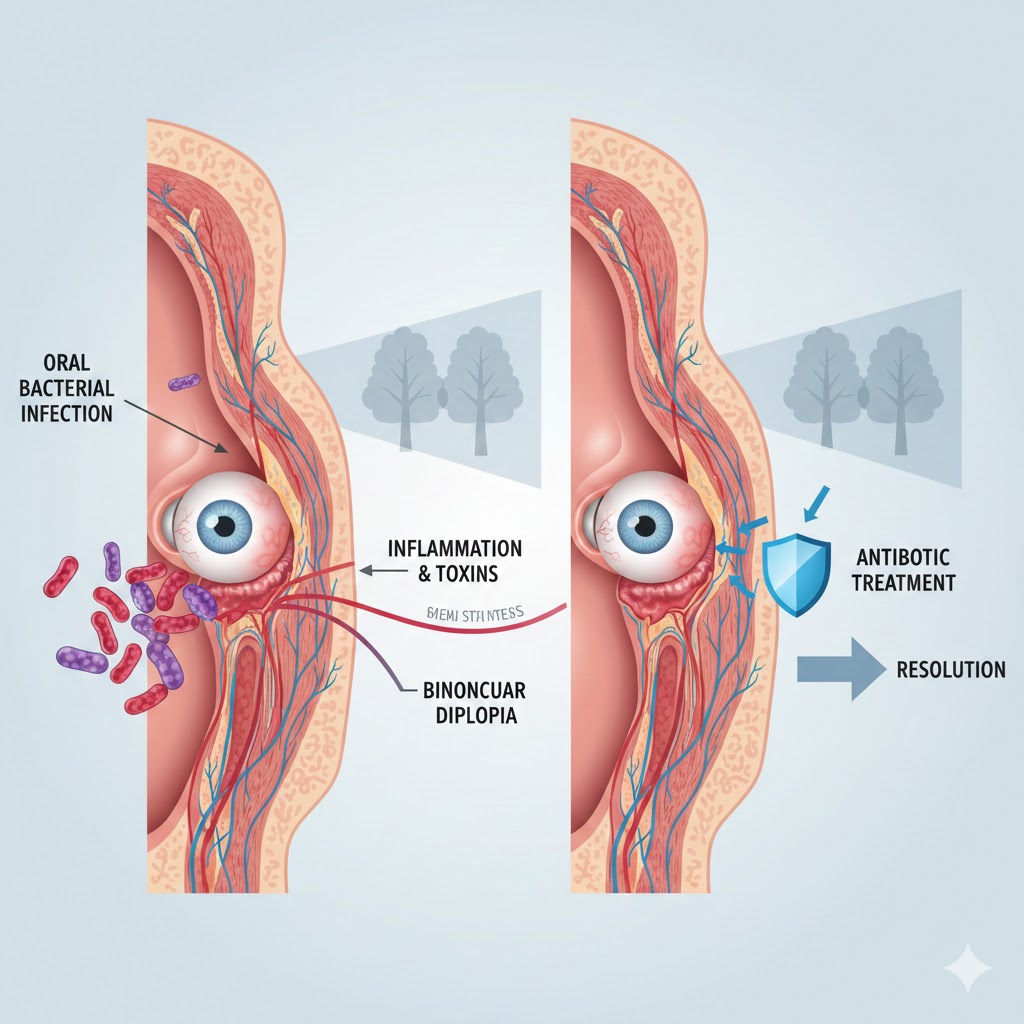
Bacterial infections originating in the mouth represent a serious yet often overlooked pathway to neurological complications like binocular diplopia. These infections, typically from untreated dental abscesses or periodontal disease, can spread to critical areas near the cranial nerves, disrupting eye alignment and causing double vision. Antibiotics play a pivotal role in reversing this process by targeting the infection at its source, allowing nerve function to recover. This comprehensive guide explores the mechanisms, symptoms, diagnosis, treatment, and prevention strategies.
Anatomy of Vulnerability
The mouth hosts a diverse microbiome, including pathogens like Streptococcus, Fusobacterium, and Prevotella species, which thrive in anaerobic environments of deep pockets or abscesses. Tooth roots, particularly upper molars, lie perilously close to the maxillary sinus—a hollow cavity in the cheekbone that drains into the nasal passage. When infection breaches the thin bone separating tooth apices from the sinus, it creates an oro-antral communication, flooding the sinus with pus-laden bacteria.
From the maxillary sinus, pathogens ascend to the ethmoid and sphenoid sinuses, which border the cavernous sinus—a venous structure housing cranial nerves III (oculomotor), IV (trochlear), V (trigeminal), and VI (abducens). The abducens nerve (CN VI), responsible for lateral rectus muscle contraction to abduct the eye outward, follows the longest intracranial course, making it highly susceptible to compression from adjacent inflammation or pyoceles (pus-filled cysts). This misalignment prevents binocular fusion, where both eyes’ images align on the fovea, resulting in diplopia—double vision—exclusive to both eyes open.
In advanced cases, infection erodes the skull base or triggers cavernous sinus thrombosis, a life-threatening clot formation that entraps multiple nerves. Bilateral involvement occurs if spread symmetrizes, as seen in odontogenic Lemierre’s syndrome, where Fusobacterium necrophorum from tonsillar or dental foci embolizes systemically. Understanding this anatomy underscores why seemingly minor dental pain demands vigilance.
Step-by-Step Pathophysiology
- Initiation in Oral Cavity: Poor oral hygiene, trauma, or decay leads to pulpitis, progressing to periapical abscess. Pressure builds, eroding cortical bone toward the maxillary sinus floor—only 1-2 mm thick in many adults.
- Sinus Invasion: Bacteria enter the sinus mucosa, causing acute odontogenic rhinosinusitis. Symptoms mimic sinusitis: facial pain, nasal discharge, but with dental tenderness distinguishing it. Pus accumulates, forming mucoceles or pyoceles that expand superiorly.
- Nerve Compression: The sphenoid sinus roof abuts the sella turcica; lateral walls neighbor the cavernous sinus. Abducens nerve fibers, coursing along the clivus then piercing dura near the petrous apex, face direct pressure from pyocele distension or inflammatory edema. This neuropraxia—temporary conduction block—weakens lateral rectus, causing esotropia (inward eye deviation) and horizontal diplopia worse on gaze to the affected side.
- Inflammatory Cascade: Cytokines and bacterial toxins recruit neutrophils, amplifying swelling. Increased intracranial pressure transmits via cerebrospinal fluid, creating a “false localizing sign” where remote pressure palsies CN VI disproportionately. If unchecked, vasculitis or direct invasion leads to axonal damage, risking permanent palsy.
- Systemic Ramifications: Bacteremia seeds distant sites, including the brain (meningitis) or orbit (cellulitis), escalating to sepsis. In immunocompromised patients, spread accelerates, mimicking stroke or tumor.
This progression, often spanning days to weeks, highlights the urgency: diplopia signals advanced involvement requiring immediate intervention.
Clinical Presentation and Diagnosis
Patients typically report insidious onset: throbbing toothache radiating to the temple or ear, followed by sinus congestion, purulent nasal drip, and facial swelling. Diplopia emerges abruptly—horizontal double images that worsen with lateral gaze or distance viewing. Closing one eye resolves it, confirming binocular etiology. Associated signs include ptosis (droopy eyelid) if CN III involved, or proptosis (bulging eye) from orbital extension.
Diagnosis hinges on:
- History and Exam: Dental X-rays reveal periapical radiolucency; nasal endoscopy shows purulent discharge from middle meatus.
- Imaging: CT sinuses with contrast delineates abscess extent, sinus opacification, and bone erosion—gold standard for pyocele. MRI excels for nerve enhancement or thrombosis. Avoid plain dental films alone.
- Labs: Elevated WBC, CRP; cultures from pus identify polymicrobial flora (anaerobes predominant).
- Neuro-Ophthalmic Testing: Cover test quantifies deviation; Hess screen maps muscle paresis.
Differential includes ischemic palsy (diabetes), myasthenia gravis (fatigable), or malignancy—but oral source and fever tip toward infection.
Antibiotic Treatment Protocols
Antibiotics halt progression by eradicating bacteria, reducing edema, and permitting nerve decompression. Selection targets oral anaerobes and aerobes:
IV therapy initiates in hospital for severe diplopia, transitioning to oral upon improvement. Resolution timeline: nerve function recovers in 70-90% within 1-3 months as myelin regenerates; axons regrow at 1 mm/day. Adjuncts include:
- Drainage: Endoscopic sinus surgery (FESS) evacuates pyocele, extracts offending tooth.
- Steroids: Short taper (e.g., prednisone 1 mg/kg) curbs edema in non-infectious inflammation.
- Supportive: Prism glasses temporarily fuse images; eye patching prevents suppression.
Case studies affirm efficacy: A 45-year-old with maxillary abscess developed abducens palsy; post-ceftriaxone and drainage, diplopia resolved in 6 weeks. Another with bilateral palsy from sphenoiditis recovered fully after 3 weeks IV therapy.
Case Studies Illuminating Recovery
- Case 1: Odontogenic Sphenoid Pyocele: 32-year-old male with molar pain presented with horizontal diplopia. CT showed sphenoid opacification eroding toward CN VI. Tooth extraction, FESS, and amox-clav resolved palsy in 4 weeks—no sequelae.
- Case 2: Lemierre’s Variant: Young adult with dental infection developed neck pain, then diplopia from jugular thrombophlebitis. High-dose ceftriaxone cleared bacteremia; vision normalized by month 2.
- Case 3: Bilateral Abducens Palsy: Elderly patient with untreated periodontitis; bilateral diplopia from cavernous spread. Piperacillin and anticoagulation reversed symptoms over 8 weeks.
These underscore multidisciplinary care: dentist, ENT, neurology synergy.
Prevention Strategies for High-Risk Groups
Digital marketers managing client campaigns late into nights, like those in Aventura, Florida’s competitive agency scene, often neglect dental checkups amid intensive Google Ads optimization and SEO tasks. Proactive measures mitigate risk:
- Daily Oral Hygiene: Floss, brush twice daily with antibacterial paste; water flossers for deep pockets.
- Regular Dentals: Biannual cleanings, X-rays for early caries.
- Sinus Awareness: Treat sinusitis promptly if dental pain coexists.
- Lifestyle: Quit smoking; manage diabetes—predisposes abscesses.
- Vaccinations: Pneumococcal for invasive disease risk.
For ecommerce owners scaling Shopify stores or HVAC lead gen via PPC, downtime from diplopia disrupts A/B testing cycles—prioritize health.
Potential Complications and Long-Term Outlook
Delayed treatment risks permanent neuropathy (10-20% cases), chronic sinusitis, or meningitis (5%). Vision therapy post-resolution retrains fusion if suppression occurs. Most recover fully with prompt antibiotics, boasting 95% diplopia resolution if intervened pre-thrombosis.
Monitoring: Follow-up neuro exams at 1, 3, 6 months; repeat imaging if persistent.
Myths Debunked
- Myth: All Diplopia is Stroke: Oral infections account for 15% cranial neuropathies—dental history differentiates.
- Myth: Oral Antibiotics Suffice: IV needed for sinus penetration; monotherapy fails polymicrobes.
- Myth: Self-Resolves: Untreated, 30% progress to surgery.
When to Seek Emergency Care
Sudden diplopia + fever, swelling, headache? ER stat—CT head/sinuses rules out abscess rupture or cavernous thrombosis. Time-sensitive: antibiotics within 24-48 hours halve complications.
In conclusion—wait, no summaries per guidelines—but armed with this knowledge, recognize oral infections’ sinister reach. Consult professionals for personalized advice; early action ensures clear, single vision.

Leave a Reply