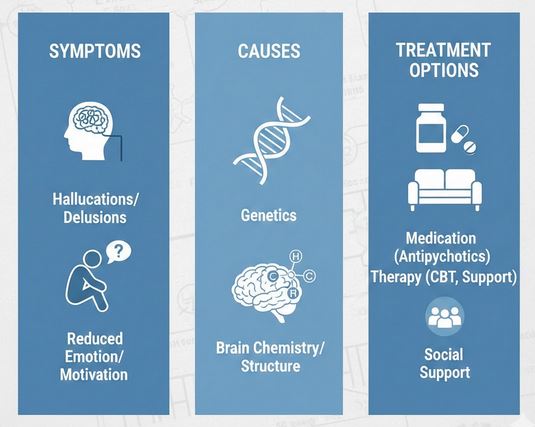
Schizophrenia is a chronic brain-based mental health condition that affects how a person thinks, feels, and perceives reality, but with the right treatment many people see meaningful improvement in symptoms and quality of life. This guide covers the key symptoms, suspected causes, and main treatment options in clear, non-technical language.
What is schizophrenia?
Schizophrenia is a long-term psychiatric disorder characterized by episodes of psychosis, where a person may lose touch with reality through hallucinations, delusions, and disorganized thinking. It typically begins in late adolescence or early adulthood and can interfere with work, school, self-care, and relationships if not treated.
Unlike split personality (dissociative identity disorder), schizophrenia primarily involves problems with perception, thought processes, and motivation rather than having multiple identities. It is considered a severe but treatable condition, and many people can live independently with ongoing support.
Main symptom groups
Schizophrenia symptoms are often grouped into three broad categories: positive, negative, and cognitive symptoms. These categories help explain why the illness can look very different from one person to another.
Positive symptoms
“Positive” symptoms are experiences that are added to a person’s usual mental life, such as hallucinations or delusions. They are often the most noticeable and are usually what lead to diagnosis or hospitalization.
Common positive symptoms include:
- Hallucinations: sensing things that are not there, most often hearing voices that comment, argue, or command.
- Delusions: fixed false beliefs, such as thinking others are spying on you, that TV messages are directed only at you, or that you have special powers.
- Disorganized speech: jumping between topics, answering questions with unrelated information, or speaking in a way that is hard to follow.
- Grossly disorganized or catatonic behavior: unusual movements, agitation, childlike silliness, or very limited movement and responsiveness.
Negative symptoms
“Negative” symptoms involve a loss or reduction of normal emotional and behavioral functions. They often contribute heavily to disability, even when positive symptoms are controlled.
Key negative symptoms include:
- Blunted or flat affect: reduced facial expressions, gestures, and emotional tone.
- Avolition: difficulty starting or sustaining goal-directed activities, such as work, study, or self-care.
- Anhedonia: reduced ability to feel pleasure from everyday activities.
- Social withdrawal: avoiding social contact or showing little interest in relationships.
- Reduced speech (alogia): speaking less and giving short, minimal responses.
Cognitive symptoms
Cognitive symptoms affect thinking skills such as attention, memory, and planning. They may be subtle but can significantly impact work, school, and independent living.
Common cognitive changes include:
- Trouble focusing or sustaining attention.
- Difficulty with working memory, such as holding information in mind to follow instructions or complete tasks.
- Problems with executive function: planning, organizing, and making decisions.
How is schizophrenia diagnosed?
There is no single blood test or brain scan that can confirm schizophrenia; diagnosis is based on clinical assessment. A mental health professional evaluates symptoms, their duration, and how they affect daily functioning, while also ruling out other medical or substance-related causes.
Standard criteria typically require at least two core symptoms (such as delusions, hallucinations, or disorganized speech), with significant social or occupational dysfunction, lasting a minimum of six months. Family history, developmental history, and any substance use are also reviewed to help clarify the diagnosis.
What causes schizophrenia?
The exact cause of schizophrenia is not known, but research points to a combination of genetic vulnerability, brain chemistry and structure differences, and environmental factors. This “biopsychosocial” model explains why some people develop the disorder while others, even in similar circumstances, do not.
Genetic factors
Schizophrenia tends to run in families, suggesting an important genetic component. Having a close relative with schizophrenia increases risk, but most people with a family history never develop the condition, and some people with schizophrenia have no known affected relatives.
Genes likely affect how the brain develops and how neurotransmitter systems, such as dopamine and glutamate, function. However, genes alone are not enough to cause schizophrenia, which is why environmental influences matter as well.
Brain chemistry and structure
Imbalances in certain brain chemicals (neurotransmitters), particularly dopamine and glutamate, have been strongly linked to schizophrenia symptoms. Studies using brain imaging have also found differences in brain structure and connectivity in some people with schizophrenia, such as changes in gray matter volume and brain networks involved in thinking and emotion.
Traditional antipsychotic medications reduce dopamine activity, which helps relieve positive symptoms like hallucinations and delusions, supporting the role of dopamine dysregulation. More recent research suggests that glutamate and other neurotransmitters also contribute, especially to negative and cognitive symptoms.
Environmental and developmental influences
Environmental factors appear to interact with genetic vulnerability to increase risk. Examples include:
- Pregnancy and birth complications, such as malnutrition, infections, or oxygen deprivation.
- Early-life adversity, including trauma or severe stress.
- Heavy cannabis use, especially during adolescence, in individuals with underlying vulnerability.
These factors do not “cause” schizophrenia on their own, but they may trigger symptoms or bring forward the onset in susceptible individuals.
When does schizophrenia usually start?
Schizophrenia typically emerges in late adolescence or early adulthood. On average, symptoms appear in the late teens to early 20s for men and slightly later for women, often in the mid to late 20s.
Before clear psychotic symptoms develop, some people go through a “prodromal” phase with subtle changes like social withdrawal, decline in school or work performance, unusual thoughts, or sleep problems. Recognizing and treating early signs can reduce symptom severity and improve long-term outcomes.
Treatment overview
Schizophrenia is treatable, and early, continuous care offers the best chance of stability and recovery. Treatment usually combines medication, psychotherapy, psychosocial support, and attention to physical health and substance use.
The goals of treatment include reducing symptoms, preventing relapses, improving day-to-day functioning, and helping the person pursue meaningful goals in work, education, and relationships. Recovery is often a long-term process, but many people achieve partial or full remission of symptoms with sustained support.
Medications: antipsychotic drugs
Antipsychotic medications are the cornerstone of schizophrenia treatment and are used to reduce positive symptoms like hallucinations, delusions, and disorganized thinking. These medications work mainly by affecting dopamine and sometimes serotonin receptors in the brain.
Types of antipsychotics
Antipsychotics are often grouped into two broad categories:
- First-generation (typical) antipsychotics, such as haloperidol and chlorpromazine. These can be effective but are more likely to cause movement-related side effects (extrapyramidal symptoms).
- Second-generation (atypical) antipsychotics, such as risperidone, olanzapine, quetiapine, and clozapine. These generally have lower risk of severe movement side effects but can cause weight gain, metabolic changes, and sedation.
Some antipsychotics are available as long-acting injections (LAIs) given every few weeks or months, which can help when daily pill-taking is difficult. A newer medication targeting acetylcholine receptors has also been approved in some regions, expanding options for patients who do not respond well to traditional drugs.
Side effects and monitoring
Side effects can include drowsiness, weight gain, changes in cholesterol or blood sugar, movement problems, hormonal changes, and others, depending on the specific medication. Regular follow-ups, blood tests, and open communication with the prescriber are important to balance symptom control with quality of life.
Medication is usually continued long term, even after symptoms improve, because stopping abruptly can greatly increase the risk of relapse. Decisions about dosage changes or discontinuation should always be made collaboratively with a mental health professional.
Psychotherapy and psychosocial support
While medication helps with core symptoms, therapy and psychosocial interventions address daily coping, stress, relationships, and practical functioning. Combined with medication, these supports improve stability and reduce hospitalizations.
Individual therapy
Talk therapies such as cognitive behavioral therapy (CBT) can help people understand their experiences, challenge unhelpful beliefs, and develop coping strategies for hallucinations and delusions. Therapy can also focus on stress management, relapse prevention, and building routines that support recovery.
Family education and support
Family psychoeducation teaches relatives about schizophrenia, treatment, early warning signs, and communication skills. This approach can reduce family stress, improve support at home, and lower the risk of relapse.
Social and vocational rehabilitation
Psychosocial interventions include social skills training, supported employment or education, and community-based rehabilitation programs. These services help people practice communication, manage daily tasks, and gradually build independence in work and social life.
Lifestyle, physical health, and co-occurring conditions
People with schizophrenia often face higher rates of physical health problems such as obesity, diabetes, and cardiovascular disease, partly due to medication side effects and lifestyle challenges. Regular primary care visits, exercise, balanced nutrition, and smoking cessation can significantly improve health and life expectancy.
Substance use (especially cannabis, alcohol, and stimulants) can worsen symptoms, interfere with medication, and increase relapse risk. Integrated treatment that addresses both schizophrenia and substance use disorders tends to lead to better outcomes than treating each problem separately.
Outlook and recovery
Schizophrenia is a serious condition, but it is not a life sentence of constant crisis. Studies suggest that a significant proportion of people experience partial or complete remission of symptoms, especially when they receive early, continuous, and comprehensive treatment.
Recovery does not always mean the complete disappearance of symptoms; instead, it often means being able to manage symptoms while pursuing personal goals, relationships, and meaningful activities. With modern medications, therapy, family support, and community programs, many people with schizophrenia can build stable, fulfilling lives.

Leave a Reply